Introduction to Past Research
Over the past 40 years, there have been many studies on the causes of SIDS and possible methods to prevent these deaths, and there has been a great deal of information gained in that effort. It appears that there are many causes of these deaths, most of which impair the infant’s ability to intake sufficient oxygen and to respond appropriately to oxygen deprivation.[3,5,7,8,10,14,17] In many of these studies, the actual sequence of events leading up to an Apparent Life Threatening Event (ALTE) or SIDS/SUID death were observed.[3,4,9] There has been an attempt to determine if monitoring could prevent these deaths based on past studies, but this has been a controversial subject with no agreement on the topic.
Success of Safe-to-Sleep Program |
Since the Safe-to-Sleep Program [13,18] (previously called the Back-to-Sleep program) was introduced in the early 1990’s, the rate of death due to SIDS has been cut in half. The Safe-to-Sleep program reduced the number of deaths by giving recommendations that would improve oxygen intake. When an infant lies on its back with no pressure on its abdomen, it takes less effort to breath. It also reduces internal breathing obstructions from the head being turned to the side. Having no blankets or soft bedding allows the infant access to fresh air and prevents re-breathing of oxygen depleted air. Not sleeping in the same bed as the parents prevents the infant from re-breathing oxygen depleted air and also prevents over-heating. Over-heating may cause an infant to fall into a deeper state of sleep where the infant may take shallower breaths and may not respond to oxygen deprivation. Having smoke-free environment prevents an infant from having problems with oxygen intake due to the smoke or to the infant’s response to a smoke environment.
The success of the Safe-to-Sleep program is a confirmation that the cause of many SIDS and SUID deaths is related the intake of oxygen.
The success of the Safe-to-Sleep program is a confirmation that the cause of many SIDS and SUID deaths is related the intake of oxygen.
The CHIME Study |
The Collaborative Home Infant Monitoring Evaluation[1] (CHIME Study) was the largest study conducted using home monitoring on infants. From 1994 to 1998, 1079 infants were monitored for a total of 718,385 hours at a cost of $25M. The purpose of the study was to determine if preterm infants, siblings of infants who died of SIDS, and infants who had experienced ALTE’s, had a higher risk of future cardio-respiratory events. The conclusion of the study was that the risk for future events, including future SIDS death, could not be predicted with monitoring.
Unfortunately, this study has been used to justify the recommendation to not monitor infants for the prevention of SIDS and SUID, which was neither the conclusion of the study, nor the purpose of the study.[2] The following are a few quotes from the CHIME study report.[1]
“The CHIME study was also not designed to determine whether use of a monitor decreases the rate of SIDS.”
“Six infants died during the study, but none was being monitored at the time of death.”
“Since many conventional and extreme events caused a monitor alarm, it is possible that the duration of some events in the risk groups was shortened by either an alarm-induced auditory arousal or by caretaker intervention.”
During the study, there were no SIDS deaths while infants were being monitored, even though there were many infants considered to be in a high risk category. The 4 SIDS deaths that did occur, occurred while the infants were not being monitored.
The study also admitted that the monitor alarm may have shortened and/or lessened the severity of the extreme events, because either the alarm aroused the infant or notified the care-giver to intervene. Even though the CHIME study does not "prove" with rigorous statistical data that monitoring can prevent SIDS deaths, it does give evidence to that effect.
Unfortunately, this study has been used to justify the recommendation to not monitor infants for the prevention of SIDS and SUID, which was neither the conclusion of the study, nor the purpose of the study.[2] The following are a few quotes from the CHIME study report.[1]
“The CHIME study was also not designed to determine whether use of a monitor decreases the rate of SIDS.”
“Six infants died during the study, but none was being monitored at the time of death.”
“Since many conventional and extreme events caused a monitor alarm, it is possible that the duration of some events in the risk groups was shortened by either an alarm-induced auditory arousal or by caretaker intervention.”
During the study, there were no SIDS deaths while infants were being monitored, even though there were many infants considered to be in a high risk category. The 4 SIDS deaths that did occur, occurred while the infants were not being monitored.
The study also admitted that the monitor alarm may have shortened and/or lessened the severity of the extreme events, because either the alarm aroused the infant or notified the care-giver to intervene. Even though the CHIME study does not "prove" with rigorous statistical data that monitoring can prevent SIDS deaths, it does give evidence to that effect.
Hypoxia and SIDS |
One of the most compelling factors from the studies is that most SIDS or SUID deaths are preceded by a lack of oxygen in the blood (hypoxia), which occurs gradually over several minutes or hours preceding the deaths.[3,4,6,9,11,12] The CHIME study also found that hypoxia preceded many of the extreme events.[15]
Frequently, the hypoxia is a repetitive condition, in which the infant recovers automatically through a mechanism know as auto-resuscitation. However, the repeated hypoxic conditions may damage internal respiratory mechanisms such that the auto-resuscitation eventually fails.
More than 90% of the SIDS deaths are a result of respiratory failure, and when respiratory failure occurs, the blood of the infant becomes deprived of oxygen. There are many reasons why infants become hypoxic, but the typical cause of death is lack of oxygen intake.[3] This is the basis for the success of the Safe-to-Sleep Program, and oxygen deprivation (hypoxia/asphyxia) is supported by numerous studies as the leading cause of death in SIDS and SUID.
Frequently, the hypoxia is a repetitive condition, in which the infant recovers automatically through a mechanism know as auto-resuscitation. However, the repeated hypoxic conditions may damage internal respiratory mechanisms such that the auto-resuscitation eventually fails.
More than 90% of the SIDS deaths are a result of respiratory failure, and when respiratory failure occurs, the blood of the infant becomes deprived of oxygen. There are many reasons why infants become hypoxic, but the typical cause of death is lack of oxygen intake.[3] This is the basis for the success of the Safe-to-Sleep Program, and oxygen deprivation (hypoxia/asphyxia) is supported by numerous studies as the leading cause of death in SIDS and SUID.
SIDS Deaths are not Instantaneous |
From several recording of SIDS deaths, it is clear that a SIDS death occurs over several minutes, and possibly hours. Indications of a pending death include hypoxic apnea, auto-resuscitation gasping, low heart rate, and low oxygen saturation in the blood (SpO2). All of these conditions can be monitored.
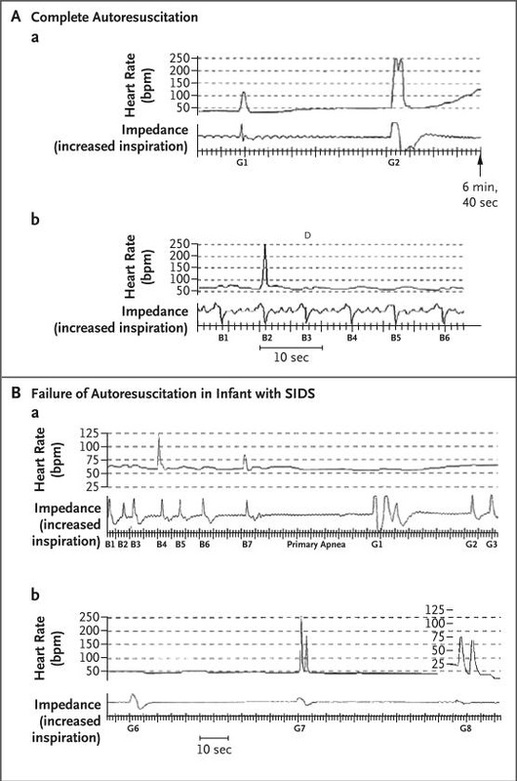
These 2 graphs are from Figure 2 in Reference 3, and show the home monitor recordings of 2 infants. In the top graph (A), the infant successfully overcomes hypoxic apnea through auto-resuscitation after 6 minutes of not breathing. The auto-resuscitation gasps are noted as G1 and G2.
In the lower graph, the auto-resuscitation failed, with the auto-resuscitation gasps noted as G1 to G8. In this case, the hypoxic apnea and repeated gasping lasted for more than 10 minutes before the heart rate finally dropped below 50 bpm, leading to the death of this infant from SIDS.
In these cases, it is clear that the conditions were not instantaneous. In the case where the infant died, there was 10 minutes of notification of a serious condition just from monitoring the breathing. It is also most likely that the SpO2 dropped long before the onset of the hypoxic apnea.
It was not explained in the article why intervention was not attempted on either of these infants.[3]
In another study [4], they found evidence of repeated full and partial auto-resuscitation events in infants who eventually died of SIDS. There has been evidence since the 1980's that hypoxia is common in infants prior to a SIDS death. [9]
Hypoxia is not an instantaneous condition. It typically develops gradually when an infant has an insufficient intake of oxygen. This can be caused by shallow breathing, obstructed breathing, re-breathing oxygen depleted air. A respiratory infection can also result in inadequate oxygen intake.
Pulse Oximetry is one method of measuring oxygen in the blood, typically giving a reading of SpO2, which is the measure of saturation of the hemoglobin in the blood, given as a percentage of maximum saturation. Generally a range of 95% to 99% is normal, but there are times when SpO2 may momentarily fall below 90%. A sustained SpO2 level below 80% to 85% is typically set as an alarm condition in a hospital.
For monitoring infants for SpO2, there has been problems with false alarms caused by motion and perfusion artifacts. The excessive false alarms of the Pulse Oximeter in the CHIME study prevented SpO2 from being used as an alarm condition. In the 25 years since CHIME monitor was designed, significant progress has been made to improve Pulse Oximetry to eliminate problems with motion and perfusion artifacts, giving a much more reliable measurement with a minimum of false alarms.
It is not clear why using today's more advanced Pulse Oximetry would not be a useful means of providing early detection of a serious condition in an infant, given that hypoxia develops gradually in most cases.
In the lower graph, the auto-resuscitation failed, with the auto-resuscitation gasps noted as G1 to G8. In this case, the hypoxic apnea and repeated gasping lasted for more than 10 minutes before the heart rate finally dropped below 50 bpm, leading to the death of this infant from SIDS.
In these cases, it is clear that the conditions were not instantaneous. In the case where the infant died, there was 10 minutes of notification of a serious condition just from monitoring the breathing. It is also most likely that the SpO2 dropped long before the onset of the hypoxic apnea.
It was not explained in the article why intervention was not attempted on either of these infants.[3]
In another study [4], they found evidence of repeated full and partial auto-resuscitation events in infants who eventually died of SIDS. There has been evidence since the 1980's that hypoxia is common in infants prior to a SIDS death. [9]
Hypoxia is not an instantaneous condition. It typically develops gradually when an infant has an insufficient intake of oxygen. This can be caused by shallow breathing, obstructed breathing, re-breathing oxygen depleted air. A respiratory infection can also result in inadequate oxygen intake.
Pulse Oximetry is one method of measuring oxygen in the blood, typically giving a reading of SpO2, which is the measure of saturation of the hemoglobin in the blood, given as a percentage of maximum saturation. Generally a range of 95% to 99% is normal, but there are times when SpO2 may momentarily fall below 90%. A sustained SpO2 level below 80% to 85% is typically set as an alarm condition in a hospital.
For monitoring infants for SpO2, there has been problems with false alarms caused by motion and perfusion artifacts. The excessive false alarms of the Pulse Oximeter in the CHIME study prevented SpO2 from being used as an alarm condition. In the 25 years since CHIME monitor was designed, significant progress has been made to improve Pulse Oximetry to eliminate problems with motion and perfusion artifacts, giving a much more reliable measurement with a minimum of false alarms.
It is not clear why using today's more advanced Pulse Oximetry would not be a useful means of providing early detection of a serious condition in an infant, given that hypoxia develops gradually in most cases.
Issues with Use of Monitors |
In the 1980s, it was speculated that monitoring could be used to prevent SIDS deaths. However, after several attempts, it was concluded that monitoring was ineffective. There were several reasons for this conclusion:
1) Early monitors were large and complex, with multiple wires that needed to be connected to the infant. This was very inconvenient, and also posed a strangulation risk.
2) Early monitors only monitored cardio-respiratory events, and did not monitor SpO2. When an infant shows signs of cardio-respiratory problems, the infant may have already suffered internal injury to the brain and cardio-respiratory system, sometimes preventing resuscitation.
3) There were many false alarms that caused stress to the parents.
4) Because of the false alarms and inconvenience of connecting the infant every time it was placed in his/her bed, there was a low compliance of using the monitors consistently.
5) There is a difficulty in training parents on the proper use of the complex monitoring system, and on how to respond to an alarm event. The cost of the monitoring equipment was high.
6) When an infant did die of SIDS, either because the monitor was turned off, or because the alarm conditions were ineffective or sounded too late, it added significantly to the “guilt” factor experienced by the parents.
7) There has been no formal study that proved monitoring is effective in preventing SIDS deaths.
It was basically concluded that the problems with monitoring, coupled with the lack of a statistically proven study, out-weighed the possible benefits of monitoring. It is now the recommendation of the American medical establishment that cardiorespiratory monitoring should not be used as a means to prevent SIDS.
Even though the CHIME study monitored 1079 infants, and the only deaths that occurred during the study were with infants not being monitored, this does not meet the standards for statistically proving that monitoring is effective. When the rate of death is only 1 in 1000 infants, to have a valid test, it would require monitoring of 5,000 to 10,000 infants. In order to conduct an effective study, the cost per monitoring hour would have to be greatly reduced compared to the CHIME study. Even so, monitoring of infants continues to be used in hospitals, particularly with preterm infants and those in intensive care units.
Important Note: There has been no physiological/medical explanation why monitoring would not be effective in preventing SIDS and SUID deaths. Many of the investigations have recommended that more studies on monitoring are necessary to determine if monitoring can be effective in preventing these deaths. In the 25 year since the CHINE study, with little reduction in the #1 cause of infant death, there has been no effective study conducted to determine if monitoring of infants would be effective. This is in spite of all the evidence supporting monitoring as a possible solution and the tremendous advancements in monitoring technology.
The current objective of the Safe Infant Sleep Foundation is to advocate for researching the effectiveness of monitoring, particularly oxygen monitoring, for preventing infant death while sleeping. It may be necessary to promote a study on the monitoring of infants to determine if monitoring can prevent many or most of these tragic and heart-breaking deaths. However, based on the evidence that lack of oxygen intake is the primary cause of many SIDS/SUID deaths, the use of pulse-oximetry monitoring devices should not be discouraged for home use.
1) Early monitors were large and complex, with multiple wires that needed to be connected to the infant. This was very inconvenient, and also posed a strangulation risk.
2) Early monitors only monitored cardio-respiratory events, and did not monitor SpO2. When an infant shows signs of cardio-respiratory problems, the infant may have already suffered internal injury to the brain and cardio-respiratory system, sometimes preventing resuscitation.
3) There were many false alarms that caused stress to the parents.
4) Because of the false alarms and inconvenience of connecting the infant every time it was placed in his/her bed, there was a low compliance of using the monitors consistently.
5) There is a difficulty in training parents on the proper use of the complex monitoring system, and on how to respond to an alarm event. The cost of the monitoring equipment was high.
6) When an infant did die of SIDS, either because the monitor was turned off, or because the alarm conditions were ineffective or sounded too late, it added significantly to the “guilt” factor experienced by the parents.
7) There has been no formal study that proved monitoring is effective in preventing SIDS deaths.
It was basically concluded that the problems with monitoring, coupled with the lack of a statistically proven study, out-weighed the possible benefits of monitoring. It is now the recommendation of the American medical establishment that cardiorespiratory monitoring should not be used as a means to prevent SIDS.
Even though the CHIME study monitored 1079 infants, and the only deaths that occurred during the study were with infants not being monitored, this does not meet the standards for statistically proving that monitoring is effective. When the rate of death is only 1 in 1000 infants, to have a valid test, it would require monitoring of 5,000 to 10,000 infants. In order to conduct an effective study, the cost per monitoring hour would have to be greatly reduced compared to the CHIME study. Even so, monitoring of infants continues to be used in hospitals, particularly with preterm infants and those in intensive care units.
Important Note: There has been no physiological/medical explanation why monitoring would not be effective in preventing SIDS and SUID deaths. Many of the investigations have recommended that more studies on monitoring are necessary to determine if monitoring can be effective in preventing these deaths. In the 25 year since the CHINE study, with little reduction in the #1 cause of infant death, there has been no effective study conducted to determine if monitoring of infants would be effective. This is in spite of all the evidence supporting monitoring as a possible solution and the tremendous advancements in monitoring technology.
The current objective of the Safe Infant Sleep Foundation is to advocate for researching the effectiveness of monitoring, particularly oxygen monitoring, for preventing infant death while sleeping. It may be necessary to promote a study on the monitoring of infants to determine if monitoring can prevent many or most of these tragic and heart-breaking deaths. However, based on the evidence that lack of oxygen intake is the primary cause of many SIDS/SUID deaths, the use of pulse-oximetry monitoring devices should not be discouraged for home use.
References |
- Coolaborative Home Monitoring Evaluation (CHIME)
- Effect of Home Monitoring on a High-Risk Population
- The Sudden Infant Death Syndrome
- Characterization of successful and failed autoresuscitation in human infants, including those dying of SIDS.
- Apparent life-threatening events: an update
- Gasping and other cardiorespiratory patterns during sudden infant deaths
- The role of respiratory control disorders in SIDS
- Tragic and Sudden Death. Potential and proven mechanisms causing sudden infant death syndrome
- Sudden Infant Death Syndrome Is Preceded by Hypoxia
- Sudden infant death syndrome (crib death)
- Competency of Autorescusitation (AR) Mechanisms in Sudden Infant Death
- SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment
- The triple risk hypotheses in sudden infant death syndrome
- Precursors of Cardiorespiratory Events in Infants Detected by Home Memory Monitor
- Reduction of motion artifact in pulse oximetry by smoothed pseudo Wigner-Ville distribution
- Sudden Unexpected Infant Death and Sudden Infant Death Syndrome
- AAP Expands Guidelines for Infant Sleep Safety and SIDS Risk Reduction
- Initial Experience and Usage Patterns With the Owlet Smart Sock Monitor in 47,495 Newborns
|
SISF Articles
|
